How Long Can You Take Gabapentin for Shingles
US Pharm. 2006;4:44-50.
Canker zoster (HZ), or shingles, is a reactivation of the varicella zoster virus (VZV or varicella) characterized by a painful rash of small blisters on a strip of skin anywhere on the body. Occasionally, the pain may continue for a prolonged period even after the rash is gone, known equally postherpetic neuralgia (PHN). Shingles is ofttimes a debilitating disease in the acute stage and even after resolution. While there is no cure, pharmacotherapy has been the mainstay of handling for shingles but may exist associated with side effects (e.g., sedation, constipation, mood swings). A new vaccination completed stage 3 trials in Apr 2005 and will probable bring hope to the many people who suffer from shingles. Until so, patient education and gimmicky pharmacotherapy will proceed to be modestly effective. The goal of this commodity is to give pharmacists a better agreement of the epidemiology, pathophysiology, clinical features, and treatment of shingles and PHN.
Epidemiology
VZV, also known as chickenpox, infects more 90% of Americans past adolescence.1 Nearly the entire population volition be infected with VZV by historic period sixty.i Reactivation of VZV later on in life produces HZ. Shingles affects 10% to 20% of the population at a rate of 131 per 100,000 individuals every yr.i A study reported that the lifetime incidence of HZ in Caucasians is twice that in African-Americans and has no preference regarding gender.2 Complications from HZ infection result in as many equally ten,000 hospitalizations and approximately 100 deaths every yr.2 Elderly individuals and people who are immunocompromised (east.g., those with HIV or AIDS), receiving immunosuppressive therapy, or have experienced a primary infection in utero or in early infancy are at high hazard for complications of HZ.1
Pathophysiology
Shingles is a neurocutaneous disease caused past the reactivation of VZV from a latent infection of dorsal sensory or cranial nervus ganglia.one Chickenpox is a highly contagious affliction, with high infection rates during childhood. VZV has the ability to establish a latent infection for the lifetime of the carrier and retains the capacity afterwards many decades to emerge at unpredictable times and cause shingles. The precise machinery of VZV reactivation is unclear just appears to be related to a diminution of host immunity or to impairment of the reticuloendothelial system that accompanies crumbling. Thus, all patients with HZ have had chickenpox in the by, fifty-fifty though the manifestation of the infection may have been extremely mild and maybe not remembered.3
HZ may involve sensory ganglia along with cutaneous nerves. The thoracic portions of the spine are virtually oftentimes affected, as followed by the lumbar and cervical portions. Viral replication of HZ spreads both centrally and peripherally along the cutaneous neuron and dorsal root ganglia. When reaching the pare, HZ replicates in the lower layers of the epidermis where it disrupts normal cellular processes. Host allowed and inflammatory responses further contribute to cellular injury.1-3
Clinical Features of Shingles
The clinical features of HZ may follow progression through three stages: prodromal, active, and chronic. Even so, information technology is common for patients not to experience all three stages. The prodromal stage seems to be the most commonly experienced. During this phase, constant or intermittent burning, tingling, itching, or diverse types of pain often precede rash past a few hours to several days. While the prodromal phase and the presence of cutaneous nervus fibrils signal that HZ infection is present in the sensory ganglia, a loss of awareness can also occur.iii
The astute phase is considered the active phase and follows the prodromal phase, which involves the evolution of characteristic skin lesions. Evolution of rash, especially in elderly patients, may exist accompanied by generalized malaise, headache, low-grade fever, and nausea. Mild encephalopathy and severe pain may too accompany these symptoms. The active phase is initially characterized past erythematous papules and edema. Papules progress to vesicles in 12 to 24 hours and to pustules within ane to 7 days. The pustules eventually dry and fall off within 14 to 21 days, leaving behind erythematous macular lesions. 1,3,4 The chronic phase is dissimilar whatsoever of the other phases and occurs mostly in the elderly. Many patients develop PHN, which is most probable to outcome during the chronic stage.1,3,four
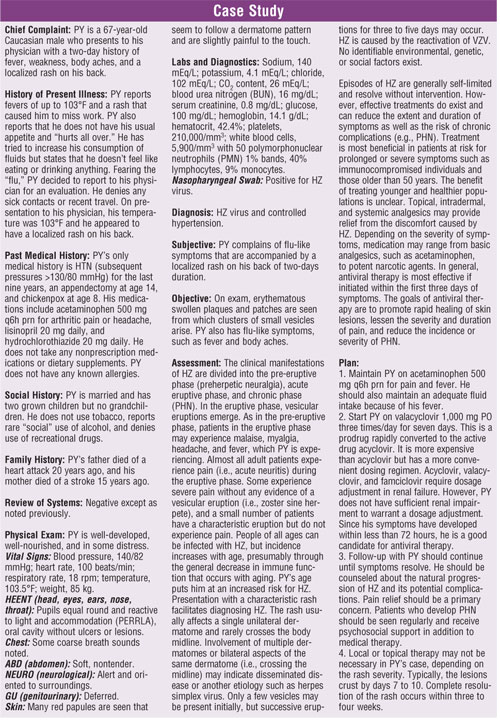
Postherpetic Neuralgia
Although the overall prevalence of PHN is 10% to 15%, virtually half of all individuals over age 70 who have experienced HZ accept had pain lasting more than one year. 4,5 Patients with PHN may take constant hurting (e.g., burning, aching, throbbing), intermittent pain (e.g., stabbing, shooting), or pain experienced subsequently a nonpainful stimulus (i.e., allodynia). These subtypes of pain may produce chronic fatigue, sleep disorders, depression, anorexia, weight loss, and social isolation. Activities of daily living, such as dressing and bathing, are oftentimes impaired in elderly patients with PHN. Less frequent chronic complications of PHN include impaired vision, hearing, vertigo, facial paresis (Ramsay Hunt syndrome), and meningoencephalitis.4,5
While the exact etiology of PHN remains unclear, it has been attributed to viral-induced edema, inflammation, and hemorrhage of the dorsal root ganglia. Neuralgia may also develop secondarily due to enhanced sympathetic vasospastic ischemia in the root ganglion.iv,6 Diagnosis of PHN is made clinically, based on the persistence of pain in a dermatological blueprint long after the vesicle eruption has healed.
Although VZV is highly contagious, information technology is generally cocky-express. Notwithstanding, if the VZV is reactivated and leads to shingles, more aggressive pain management, symptomatic relief and, occasionally, antiviral agents may be used in treatment.
Direction of Shingles
A combination of nonpharmacologic therapy and medication is the most constructive approach for managing HZ. Education about the illness may aid eliminate anxiety and fear associated with the disease. Social support, acceptable rest and physical activity, proper nutrition, and local therapy can help manage HZ. Pharmacologic approaches include the use of antiviral therapy, antidepressants, anti-inflammatory agents, anticonvulsants, and systemic and topical analgesics individualized to each patient'south needs.vi,seven Neuropathic pain may be unresponsive to opiates. Some patients with PHN will do good from elementary analgesics, such as acetaminophen and NSAIDs.
Antiviral Therapy:
Therapy with antiviral agents can reduce the pain of acute PHN and help with the healing process. A recent review article found that when initiated inside 72 hours of rash onset, oral acyclovir decreases the incidence and severity of neuropathic hurting.eight Antiviral agents may be benign while new lesions are actively being formed just are unlikely to be helpful afterward lesions have crusted.viii Yet, the effectiveness of antiviral agents in preventing PHN is under debate; numerous studies have been conducted, merely the results take been variable. The approved dose of acyclovir for the handling of shingles is 800 mg 5 times/day for seven to 10 days. The newer analogs of acyclovir, such as famciclovir (Famvir/Novartis) or valacyclovir (Valtrex/Glaxo), may likewise be used and only demand to exist administered two to four times daily. Compliance to acyclovir may be difficult since five doses per twenty-four hours are required.vi-8 All antivirals must exist initiated within 72 hours, and ideally, within 24 hours, to be constructive.
Tricyclic Antidepressants:
Tricyclic antidepressants (TCAs) are considered the mainstay of therapy for PHN, although their side effects limit their usefulness. While their mechanism is unclear, TCAs inhibit central nervous arrangement reuptake of norepinephrine and serotonin and may increase the inhibition of nociceptive signals from the periphery. In a study that compared amitriptyline to lorazepam in the handling of PHN, amitriptyline demonstrated moderately significant pain relief over lorazepam.7,8 Withal, due to the overwhelming anticholinergic side effects of TCAs (i.e., dry mouth, urinary retention, blurry vision, and constipation), they are non recommended in the elderly. A typical initial dose of amitriptyline for neuropathic pain is 25 mg at bedtime, which may be slowly increased every bit tolerated to 100 mg/day. Less anticholinergic TCAs, such as nortriptyline, may be preferred since they are better tolerated than amitriptyline.
Corticosteroids:
Systemic corticosteroids are the therapies most widely recommended by dermatologists to control cutaneous eruptions and pain.8 While several different routes of administration take been studied in the acute stage of PHN, oral corticosteroids appear most useful. Oral prednisone forty mg daily tapered over three weeks, decreasing by 10 mg weekly, is effective at reducing the elapsing of HZ and associated symptoms. Notwithstanding, additional studies have found that the benefits of corticosteroids in patients older than lx years is questionable, and adjuvant therapy such as antivirals should be used concomitantly.7,viii The side effects of systemic corticosteroids such as prednisone should exist familiar to pharmacists. Short-term adverse reactions include mood swings, hyperglycemia, appetite changes, and hypokalemia (arising from mineralocorticoid activity). Chronic steroid therapy may be associated with adrenal suppression, impaired wound healing, cataract formation, skin thinning, and osteopenia or osteoporosis. Since the adventure of side effects increases with the dosage and duration of steroid therapy, patients should be maintained on steroids just as long as clinically necessary.
Gabapentin:
The anticonvulsant gabapentin (Neurontin/Pfizer) is approved for the handling of PHN. The drug works by reducing spontaneous neuronal firing through membrane-stabilizing furnishings. Anticonvulsants were originally introduced for the treatment of epilepsy but accept been constitute to exist useful for neuropathic pain. In a randomized, double-blind, placebo-controlled study, gabapentin was effective in the treatment of hurting and sleep interference associated with PHN.ix Patients' mood and quality of life by and large amend with gabapentin therapy. Gabapentin is associated with a diversity of side furnishings, including sedation, dizziness, somnolence, and memory disturbances. Rare adverse effects with gabapentin include liver toxicity and thrombocytopenia. The dosage for gabapentin for the treatment of PHN is every bit follows: twenty-four hours 1, 300 mg; day 2, 300 mg two times/day; and day 3, 300 mg iii times/day. The dose may be titrated to between 1,800 and 3,600 mg/day equally needed for hurting relief. Daily doses greater than 1,800 mg do not generally show increased benefit.
Capsaicin:
The topical analgesic capsaicin is thought to produce analgesia by depletion of substance P, a nocigenic peptide associated with pain. Topical application of capsaicin tin crusade burning and erythema, only has been found to produce moderate relief when applied iv times daily.10,11 The recommended force of capsaicin is 0.075% (Zostrix HP/Rodlen Laboratories), and it must be applied directly to areas of pain three to iv times daily. Patients should be instructed to article of clothing gloves when applying the medication, launder hands immediately afterward application, and discontinue use if astringent burning or intense itching occurs.
Transdermal Lidocaine:
Lidocaine 5% patch (Lidoderm/Endo Pharmaceuticals) is also useful for local pain associated with PHN. The patch may remain in place for upward to 12 hours, and upwards to three patches may be applied in a single application in whatsoever 24-hour flow. The about common side effects of lidocaine are skin redness or rash.
Prospects for Shingles Vaccination
The morbidity of HZ could exist reduced if a safe and constructive preventive handling were available. Zostavax (zoster vaccine live/Merck) is an investigational shingles vaccine. In a recent placebo-controlled clinical trial, the vaccine reduced the total brunt of pain and discomfort caused by shingles past 61%, the incidence of PHN by 67%, and the overall incidence of shingles cases by 51%. 12 The study was conducted in more than 38,500 men and women ages 60 years and older. Participants were enrolled from 1998 to 2001, with the follow-up completed in 2004. Enrollment criteria included history of chickenpox (varicella) or residency in the U.s. for more than than 30 years. Patients were excluded if they were immunocompromised or unable to attach to the specific requirements of the protocol. More 95% of participants completed the written report.12 The rates of serious adverse events were low, and the number and types of serious adverse events were similar in the vaccine and placebo groups. Erythema and rash effectually the injection site were common agin effects.
Decision
Shingles is oft a confusing and frustrating illness, especially for patients. Electric current treatment options focused on relieving the symptoms of PHN include TCAs, analgesics, anticonvulsants (gabapentin), and topical agents such as capsaicin and lidocaine. Since shingles often affects elderly patients, it is particularly important that pharmacists be enlightened of the adverse effect profile of these medications. Pharmacists should educate patients and advise them if drug interactions are anticipated or if adverse effects are suspected. Baseline pain intensity and the nature of pain (eastward.g., tingling, called-for) should be used to assess the effectiveness of pharmacotherapy for PHN. Although the management of shingles is primarily symptomatic and supportive, since antivirals may not reduce the incidence of the disease, HZ vaccination holds promise for the future.
REFERENCES
1. Mullooly JP, Riedlinger Yard, Chun C, et al. Incidence of canker zoster, 1997-2002. Epidemiol Infect. 2005;133:245-253.
2. Schmader KE, Dworkin RH. Handling and prevention of postherpetic neuralgia. Clin Infect Dis. 2003;36:877-882.
3. Nicholson BD. Diagnosis and management of neuropathic pain: a balanced approach to treatment. J Am Acad Nurse Pract. 2003;15(12 suppl):3-nine.
4. Pearce JM. Postherpetic neuralgia. J Neurol Neurosurg Psychiatry. 2005;76:572.
5. Argoff CE, Katz Northward, Backonja G. Treatment of postherpetic neuralgia: a review of therapeutic options. J Pain Symptom Manage. 2004;28:396-411.
half-dozen. Hampton T. When shingles wanes but hurting does non: researchers target postherpetic neuralgia. JAMA. 2005;293:2459-2460.
7. Johnson RW. Pain post-obit herpes zoster: implications for management. Herpes. 2005;11:63-65.
8. Watson CP. Management issues of neuropathic trigeminal hurting from a medical prospective. J Orofac Pain. 2004;18:366-373.
ix. Parsons B, Tive L, Huang S. Gabapentin: a pooled analysis of adverse events from three clinical trials in patients with postherpetic neuralgia. Am J Geriatr Pharmacother . 2004;ii:157-162.
10. Barger A, Dukes E, McCarberg B, et al. Change in opioid use after the initiation of gabapentin therapy in patients with postherpetic neuralgia. Clin Ther. 2003;25:2809-2821.
11. Hempenstall K, Nurmikko TJ, Johnson RW, et al. Analgesic therapy in postherpetic neuralgia: a quantitative systemic review. PLoS Med. 2005;two:164.
12. Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to foreclose herpes zoster and postherpetic neuralgia in older adults. Northward Engl J Med. 2005;352:2271-2284.
To comment on this commodity, contact editor@uspharmacist.com.
Source: https://www.uspharmacist.com/article/what-pharmacists-need-to-know-about-shingles
0 Response to "How Long Can You Take Gabapentin for Shingles"
Enregistrer un commentaire